Table of Contents
Overview
Definition
Assessing Obsessive-Compulsive Disorder: The Y-BOCS Test
OCD: A Condition with Anxiety at Its Heart
Obsessive-Compulsive Disorder in the Public Eye
Obsessive-Compulsive Disorder Treatments
OCD Support Communities
OCD-Based Anxiety During Widespread Health Emergencies
Overview
Obsessive compulsive disorder, or OCD, is an anxiety-based mental health condition that affects many individuals across the globe. The disorder enhances more familiar fears and concerns by turning one’s attention to stress-inducing triggers.
Despite a growing percentage of individuals diagnosed with OCD, this condition can oftentimes be overlooked, having a detrimental effect on one’s well-being. As with other brain disorders, equipping yourself with knowledge about the background, symptoms and available OCD treatments plays a crucial role on your road to a better quality of life.

What is Obsessive Compulsive Disorder?
Obsessive-compulsive disorder is a mental health disorder defined by a combination of anxiety-causing thoughts and behaviors.
OCD disrupts an individual’s sense of well-being by acting like an overactive defense mechanism: under OCD, somewhat concerning stimuli (e.g. tracking dirt inside your house) can bring about a great deal of anxiety. This can lead the individual to focus their thoughts on the stressor that triggered their distress and try to calm themselves down by carrying out a certain pattern of behavior (e.g. washing their shoes). Unfortunately, OCD-related actions often end up doing the opposite (e.g. cleaning one’s shoes is perceived as having “infected” the rag you used to clean them with, your hands and overall body), thereby feeding your anxiety in a continuous loop.
Obsessive Thoughts
Though there are endless examples of OCD-related thoughts, the more common ones can be divided into four categories, appearing either on their own or together with one another:

Contamination or cleanliness concerns (e.g. picking up an illness from touching a door handle).

Worry over disaster striking (e.g. taking a different way to work may end up in a car accident).

A focus on symmetry, organization, counting, or “just right” thinking (e.g. folding and refolding your laundry until every item is “perfectly” neat).

Taboo or “immoral” thoughts and rituals (e.g. having a violent thought about causing harm to someone you care about).
OCD-related thoughts are experienced as unwanted, intrusive, and greatly distressing. They can severely impair an individual’s daily life and cause them a substantial amount of worry, guilt or frustration.
Compulsive Behavior
OCD-related compulsions are the actions the individual carries out in an effort to quell their rising anxiety. Despite this initial motivation, the compulsive behavior that arises ends up increasing the level of experienced anxiety, while also negatively affecting the individual’s physical, mental, social, and emotional well-being.
Examples of OCD-related compulsive behaviors are varied and may include constant hand-washing, repeatedly making sure your gas stove is safely turned off, rearranging your bookshelf to fit a perceived “ideal” order, or trying to dispel a distressing thought about a loved one falling in harm’s way by repeating the same hand gesture.
Such compulsive actions are performed to achieve a momentary relief, but in the long run fail to actually ward off obsessive thoughts. As they go through repeated, OCD-related behavior, many individuals start contending with self-doubt: did they really turn off the lights four times as they meant to do, or did they miss one? Did they remember to wash both of their thumbs, or not? To be on the safe side, they repeat their action once more, and then again, until they can be sure they have carried it out flawlessly. Such actions quickly become an exhausting, energy-depleting and extremely frustrating ritual, all without alleviating the OCD-related anxiety that triggered them.

An individual dealing with obsessive compulsive disorder can experience obsessive thoughts or compulsive behaviors, without necessarily having to contend with both. Regardless, both OCD-related thoughts and behavior impede upon the individual experiencing them, and end up exacerbating one another. OCD symptom severity and frequency can also grow as the disorder continues, adding to the individual’s frustration over their condition.
Insight and Tic Disorder Specifiers
In addition to noting symptoms of obsessive thoughts and compulsive behaviors, an OCD diagnosis includes two specifiers: assessing the individual’s level of insight into their condition, and whether they also have a tic disorder. A patient’s insight attests to how aware they are that they are suffering from OCD, with the vast majority of patients—over 96%—falling between “good or fair insight” to “poor insight.” In fact, many OCD sufferers may rationalize their thoughts or behavior as personality quirks, unworthy of diagnosis or treatment. The existence of a tic disorder, referring to sudden involuntary twitches, movements, or sounds that are performed repeatedly, is also considered, since over 30% of individuals with OCD also face a tic disorder.
OCD-Related Disorders
Obsessive compulsive disorder is actually included among a range of what is referred to in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (or DSM-V) as OCD-related disorders, which are also known as OCD-spectrum disorders. The conditions in this group include disorders that, like OCD, involve an obsessive thought pattern combined with an unwanted action or ceremony intended to ward off feelings of anxiety.
OCD-related disorders include the following:
Body dysmorphic disorder: A preoccupation with a perceived or minor physical flaw, body dysmorphic disorder causes the individual to carry out repeated actions (e.g. looking in the mirror) or mental acts (e.g. comparing their appearance to others’). Individuals with this condition will often seek out numerous cosmetic procedures to try to improve their perceived physical flaw. While many of the symptoms are similar to those of eating disorders, patients diagnosed with BDD does not necessarily involve considerations of eating or weight.
Hoarding: A difficulty throwing away or parting with physical items, regardless of their actual value, due to a strong perceived need to save them and feelings of distress at the thought of discarding them. Hoarders often have little insight into the severity of their condition, even when their home is no longer a livable space and social or family relationships are damaged.
Excoriation: Characterized by picking one’s skin to remove perceived or actual small irregularities, leading to skin lesions.
Trichotillomania: Defined by repeatedly pulling out of one’s hair, which may result in eventual hair loss.
Substance/Medication-Induced Obsessive-Compulsive and Related Disorder: Consists of obsessive-compulsive symptoms that are due to substance intoxication, withdrawal or relating to medication.
Obsessive Compulsive and Related Disorder Due to Another Medical Condition: Obsessive compulsive symptoms linked to OCD and related disorders that do not amount to an official diagnosis.
While not an OCD-related disorder, PANDAS, or Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections, are a group of conditions unique to children, in which OCD or a tic disorder suddenly develops or becomes exacerbated following strep throat or scarlet fever.
Prognosis and Epidemiology
2.3% of US adults and 1%-2.3% of US children and adolescents will contend with OCD. These statistics do not include the many individuals who face subclinical OCD, due to not meeting the requirements for an official OCD diagnosis.
OCD can develop at any age, with symptoms commonly appearing between the age of ten and early adulthood. Despite this, on average patients are only diagnosed and begin receiving treatment from ages 14-17. This is because OCD can be challenging to diagnose, and can often be rationalized as a personal eccentricity, rather than an official mental health condition.

Demographics and Risk Factors
The following risk factors increase the probability of developing OCD:
Gender: It remains unclear what role (if any) gender plays in OCD. While the European-based International Classification of Diseases (ICD-10) health manual has found OCD prevalence to be roughly the same among women and men, the American-based DSM mental health manual has found women to be slightly more affected than men during adulthood, and boys to be more affected girls during childhood. The DSM also notes that women with OCD are more likely to develop cleanliness-related OCD, while men with OCD are more likely to develop forbidden thoughts and symmetry-related OCD, as well as a tic disorder.
Age: The age and life phase of an individual with OCD have been shown to influence the type of thought content they fixate on. Children and adolescents obsess more over possible catastrophes or hurting others, with adolescents also reporting more sexual and religious-focused OCD.
Anxiety and Depression Disorders: Individuals with OCD have a higher tendency to develop anxiety and depression disorders, as well. Roughly three in four have a lifetime history of anxiety disorders, and close to one in two also contend with depression.
Suicidality: Up to a quarter of those with OCD have reportedly attempted to take their own lives. The risk of suicidal ideation also increases in the presence of major depressive disorder (MDD).
Cultural Factors: OCD has been extensively researched within a variety of cultural contexts. Findings have concluded that this condition is not more common in certain cultures, nor does culture seem to determine the age an individual is more likely to develop OCD.
Hoarding: Hoarding also increases the chances of developing OCD. When found together, both of these conditions often feed a fear that not performing a certain act (OCD-related behavior or discarding an item) will lead to a loved one falling into harm’s way.
Assessing Obsessive-Compulsive Disorder: The Y-BOCS Test
Diagnosing OCD is normally carried out by psychiatrists who specialize in this field. To determine the existence and severity of an individual’s OCD, they rely on assessment tools, most commonly the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS). The Y-BOCS helps consider an OCD diagnosis through the following parameters, which detail the level of awareness, negative impact on their mental health, and the individual’s current ability to resist their OCD-related symptoms:

The existence of specific OCD symptoms.

The amount of time they spend on OCD-related obsessions or compulsions.

The degree to which their OCD interferes with their life.

The level of distress it causes them.

The degree of control they have over their OCD-related thoughts.

How able they are to resist carrying out OCD-related compulsive behavior.
OCD: A Condition with Anxiety at Its Heart
These days, obsessive compulsive disorder receives a great deal of focus as a standalone condition, and its own separate section in the two major diagnostic manuals—the American Psychiatric Association’s DSM-V and the World Health Organization’s ICD-10. However, this was not always the case, as OCD was originally grouped together with other anxiety-based conditions.
Grouping OCD under the anxiety umbrella made sense, as anxiety is OCD’s central and most disturbing symptom. As such, understanding OCD at its core necessitates a better understanding of its main symptom.
Anxiety is perceived as a system overload, with the individual adversely and overly worried about dangers whose probability remains unclear. In the case of OCD, this overly reactive fear is directed at mundane factors, such as dirt or clutter, making them unbearable for the patient.

Why Separate OCD from Anxiety?
Removing OCD from the anxiety family, while focusing a great deal of research and visibility on OCD, has raised criticism from mental health experts. Specifically, detractors have pushed for anxiety, and not OCD, to receive more attention, since anxiety disorders are found in a much larger percentage of the population: 19.1% of US are diagnosed with an anxiety disorder, and 31.1% of US adults will have dealt with it at some point in their lives. This compared to 1.2% of US adults having faced OCD over the past year, and 2.3% of US adults having faced it over their lifetime.
That said, certain key discoveries have justified OCD’s more recent place in the spotlight. Researchers’ increased understanding of this condition has already uncovered which neural pathways and structures play a part in the development of OCD, as well as what treatments have proven to offer patients symptom relief. OCD-focused research has additionally found unique familial, genetic, and neural commonalities among OCD and OCD-related disorders that further distinguish them from other anxiety-based disorders.
Obsessive-Compulsive Disorder in the Public Eye
The steady rise in OCD’s visibility is certainly tied in part to the above-mentioned advances in clinical research. But in addition to science, another factor has helped turn society’s focus in OCD’s direction: popular culture.
OCD seems to have captured popular imagination due to the many ways it relates to aspects of everyday life. Several OCD symptoms, mainly a focus on cleanliness, efficiency, and organization, are often portrayed in entertainment news outlets as “quirky OCD traits,” instead of aspects of a debilitating mental illness. Such depictions run the risk of flippantly describing a serious affliction as a personality flaw, adding to the rate of OCD misdiagnosis.
Increased public interest in OCD does, however, also has a positive side. Many news outlets take a more respectful approach when discussing experiencing OCD, making the subject more accessible to their readers. This in turn helps combat mental health stigma and raise awareness of available treatment options.
In addition, numerous celebrities have gone public with their struggle with OCD, including Justin Timberlake and Daniel Radcliffe, bringing additional awareness to the condition. As another example, an article by ESPN reporter Jackie MacMullen brought to light the struggle of numerous NBA athletes to cope with their OCD symptoms and the increased focus of the league to provide access to treatment.
Obsessive-Compulsive Disorder Treatments
There is a growing number of OCD treatment options available these days. Many of them can be combined as part of an overall treatment course, though it is important to consult your mental health provider before deciding which options you should try. OCD Medical Device Treatment
Deep TMS: The only non-invasive medical device that is FDA-cleared with published clinical efficacy data to treat OCD, Deep Transcranial Magnetic Stimulation, or Deep TMS, utilizes magnetic fields to safely regulate the neural activity of brain structures such as the anterior cingulate cortex, which have been found to be associated with OCD. The treatment’s effectiveness was reaffirmed in a 2019 multicenter study published by the American Journal of Psychiatry. Specifically, the study found that Deep TMS’s regulating the neural functions of “the medial prefrontal cortex and anterior cingulate cortex significantly improved OCD symptoms.”

Deep TMS is actually an advancement of standard TMS that addresses some of the issues raised by its predecessor, which has granted Deep TMS its aforementioned FDA clearance status. Both are non-invasive treatments that rely on a magnetic field to regulate neural functioning.
Unlike the figure-8 design used by standard TMS, Deep TMS uses its own patented H-Coil technology, held inside a cushioned helmet fitted onto the patient’s head. The magnetic fields produced by the H-Coil manage to safely reach wider regions of the brain, and can directly stimulate deeper brain structures than standard TMS.

Deep TMS does not cause any adverse or long-lasting side effects, the most common being a local and passing headache. Furthermore, as a non-invasive treatment, Deep TMS can be combined with other forms of treatment when treating OCD.
OCD Medication Treatment: Efficacy Counterbalanced by Side Effects
Several psychiatric medications have been shown to offer symptom relief for patients with OCD. Five types of medication have been FDA-approved to treat this condition. Out of the five medications FDA-approved for treating OCD, four are selective serotonin reuptake inhibitors (SSRIs) and one is from the tricyclics (TCA) family.
Though many patients report a reduction in symptom severity and frequency when taking them, OCD medications have also been known to cause possible side effects.
SSRIs: Selective serotonin reuptake inhibitors are presently considered to be a first-line obsessive-compulsive disorder treatment, in addition to cognitive behavioral treatment (CBT). The medications included in this family keep the neurotransmitter serotonin active for a longer time, which increases its efficacy. Current FDA-approved SSRIs for OCD include sertraline (Zoloft), fluoxetine (Prozac), fluvoxamine (Luvox) and paroxetine (Paxil).
SSRIs are more commonly known as antidepressants, and are also a very popular treatment for major depressive disorder. However, SSRIs and in fact all antidepressants are also considered anxiolytics, due to their ability to inhibit anxiety, in addition to depression. Since OCD is an anxiety-centered disorder, SSRIs were eventually found to help alleviate OCD symptoms, as well.
But while SSRIs are considered effective and relatively well-tolerated, some patients find their accompanying side effects to be adverse, and discontinue treatment as a result. Weight gain, nausea and sexual dysfunction are among their more common side effects.
In addition, 40%-60% of patients with OCD show little-to-no symptom improvement from first-line medication. As a result, many patients continue searching for a treatment option that works for them.
Clomipramine: The tricyclic medication clomipramine is considered a second-line treatment for OCD, and was more frequently prescribed to treat this condition during the ‘80s. This medication works to prevent the reuptake process of both serotonin and norepinephrine. Due to its more severe side effects, these days clomipramine is less frequently prescribed.
Psychotherapy for OCD: Proven Results at Lower Risk
Psychotherapy, or talk therapy as it is sometimes referred to, offers patients the chance to gradually enter into a therapeutic process that acknowledges not only their symptoms, but the larger life context in which they have evolved.
Four branches of psychotherapy are considered to be the most effective when treating OCD: cognitive behavioral therapy, psychodynamics, exposure and response prevention therapy, and acceptance and commitment therapy.

Cognitive Behavioral Therapy: Another first-line OCD treatment, CBT is a type of psychotherapy that has shown to be particularly effective with this disorder. The treatment helps identify the emotions, thoughts, behaviors and physical reactions that are associated with a patient’s OCD. Recognizing the different aspects of their condition can help patients understand it better, become less anxious when experiencing its symptoms, and eventually consider new modes of response.
Psychodynamics: A more reflective form of therapy, whose results may be slower to develop, psychodynamics offers a deep dive approach to OCD. It focuses on the interactions between formative ties and relationships, crucial life events, central needs and desires, powerful automatic beliefs and specific personality traits, as a means to understand what factors contributed to the development of OCD. After uncovering the relevant factors, the therapist and patient duo work together to loosen the rigid, maladaptive patterns that have preserved the patient’s OCD symptoms. Eventually, the patient is hopefully able to consider more beneficial alternatives that can offer them relief and strengthen their sense of well-being.
Exposure and Response Prevention Therapy: ERP utilizes exposure techniques to desensitize patients when faced with triggering stimuli. ERP gradually exposes the patient to the perceived source of their anxiety, as their therapist accompanies and offers them support, while helping the patients avoid acting out their compulsions. ERP is thought to help patients develop a more durable approach to their intrusive, adverse thoughts, as they overcome their compulsive reactions to them in situations that are external to the therapeutic setting.
Acceptance and Commitment Therapy: ACT approaches OCD by emphasizing psychological flexibility in regard to OCD-related obsessive thoughts. It also underscores how a patient’s commitment to their therapeutic journey has the power to create behavioral change.

Invasive OCD Treatments: Still Much Left to Learn
Invasive obsessive-compulsive disorder treatments as a whole, and particularly neurosurgical ones, are still being studied to determine their safety and efficacy. They normally necessitate a recovery period, with research on these forms of therapy largely limited to small numbers of patients. As such, invasive OCD treatments are normally only considered after less invasive, first-line options have been exhausted.
Recent studies on neurological lesion methods have shown potential in their ability to alleviate OCD symptoms for treatment-resistant patients. These methods include standard craniotomy, gamma knife coagulative lesions, and implanting radioactive seeds that induce local ablations. Most ablative, neurosurgical options are carried out on the brain’s cortico-striato-thalamo-cortical circuit, which is thought to become hyperactive in patients facing OCD.
OCD Support Communities
Patients with OCD can struggle with their condition on a daily basis and can greatly benefit from belonging to a support network that offers them a forum to share and acknowledge each other’s experiences.
In addition to individual therapy and the support of loved ones, local group therapy meetings are an option in many areas of the world. The International OCD Foundation is a reliable source of information when it comes to support communities, in addition to general information about OCD. An additional option is social media platforms, which provide designated forums and personal channels on which you can connect with other individuals contending with OCD.
OCD-Based Anxiety During Widespread Health Emergencies
As a mental health condition centered on anxiety, OCD can cause significant distress even during periods of general tranquility. When faced with circumstances that trigger their OCD, individuals contending with this disorder are even more likely to suffer from it, as is the case when dealing with a vast health crisis.
This is particularly true for individuals with cleanliness-based OCD facing a global pandemic like COVID-19. The close attention being paid to sterilization, hand-washing and avoiding the possibility of infection are all extremely triggering for their condition, and act to highlight the very concerns that have taken over their lives.
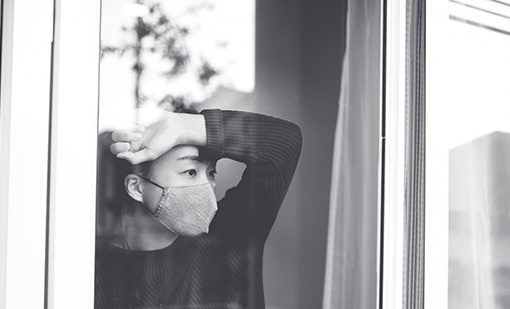
Having the world at large hyper-vigilant regarding the possibility of infection can undermine any progress patients with cleanliness-themed OCD may have achieved. Indeed, as a result of conflicting demands between managing their OCD and adhering to the greatest level of sanitation, patients with OCD are reportedly experiencing increased levels of health-related anxiety.
Many of those contending with anxiety-based conditions, such as cleanliness-focused OCD, view global health crises as a real-life manifestation of their most powerful fears. Having access to an effective treatment course, as well as receiving the necessary empathy and support from their environment are all crucial components in their battle to securely withstand the challenges that come with this condition, in times of crisis and throughout their lives.


Comments